Risk of Developing Diabetes in Individuals With Family History of Diabetes
In this lecture honoring Professor Stefan S. Fajans of the Academy of Michigan, I am going to address iv major topics related to diabetes:
- [a]
Statistics about the global diabetes epidemic : facts and fallacies;
- [b]
Epidemiological information nearly the diabetes epidemic: secular rises and falls;
- [c]
The drivers of the blazon 2 diabetes epidemic; and
- [d]
Epigenetics and early on life exposure of the fetus that may influence the risk of diabetes in adult life.
The Black Decease was ane of the near devastating pandemics in man history, killing as much equally 20% of the earth's population in the 14th century [1]. But that was then. In the 21st century, the question may be asked, is blazon 2 diabetes the biggest epidemic in history? I believe it is a much bigger epidemic than the Black Death and in this talk I will endeavour to prove it to you.
Statistics about the global diabetes epidemic: facts and fallacies
The International Diabetes Federation (IDF) has asked a very simple question, if you look at the world'southward nearly populous countries, where would diabetes fit? Numerically diabetes, if it were a nation, would surpass the United States every bit the third most populated land in the earth. While there are approximately 320 million people in the U.S., at that place are at present 415 1000000 people in the world with diabetes co-ordinate to the IDF [2]. This is clear evidence to suggest that nosotros have a major global problem with type 2 diabetes.
The IDF has attempted to create awareness of the importance of blazon two diabetes. In the year 2000, IDF estimated there were 151 million people with diabetes globally and predicted that by 2030, there would exist 324 meg people in the globe with diabetes [iii]. The World Wellness Organisation (WHO) also estimated the global prevalence of diabetes in 2000 and 2030–171 meg people with diabetes in 2000 and 366 million by 2030 [iv]. They were terribly wrong, because by 2015 there were already 415 million people with diabetes, far above what was predicted in 2000 for 30 years after. And the state of affairs may even be worse than that. To perform its global projections, the IDF estimates how many people have diabetes in each state. If a country does non take data about diabetes prevalence, the IDF extrapolates from another country using regional data [3] or match geography, World Banking company income, ethnicity and language [2]. These extrapolations are less reliable. If anything, the current IDF estimates are withal a quite serious underestimate.
This upshot is of more than academic interest because young researchers in epidemiology may call back the IDF and WHO data are gospel. Unfortunately, they may represent a quick catch of data that become out for public relations purposes and non necessarily for public health benefit and planning.
In 1978, a Kroc Foundation International Conference on Epidemiology of Diabetes and Its Macrovascular Complications was held in Santa Ynez Valley, California. Attendees included Kelly W, Peter Bennett, Harry Dandy and other legendary figures in diabetes epidemiology. I was also there, though as a "budding" epidemiologist! The Santa Ynez Valley meeting produced a nomenclature of diabetes, diagnostic criteria, and proper protocols for diabetes epidemiology studies [v], so if a study was done in Japan, it would exist comparable to one performed in the Usa. This heritage of consensus and standardization has been lost of late because of the practice of the IDF and WHO and indeed the Global Burden of Disease Group [6] and others to publish data which underestimate the burden of diabetes and, if used for public health purposes, probably underestimate the resources required to attack the epidemic. So we accept issued a word of caution and hopefully the give-and-take will get out [6].
The WHO is at least, in part, at fault in this, as they support the STEPS program which diagnoses diabetes based on the fasting glucose level alone [7]. Notably, Stefan Fajans and Jerome Conn did non even include the fasting glucose in their criteria for the oral glucose tolerance exam [8]. Whether they were wise or it was an oversight on their part, I cannot say, but nosotros know the measurement of fasting glucose alone underestimates the prevalence of diabetes past 20–25% [ix].
If epidemiologists of policy makers apply country-specific estimates provided by IDF or WHO for their planning, they should carefully examine the appropriateness of whatever extrapolation of data from one country to another and evaluate the criteria used to diagnose diabetes. Inappropriate extrapolations and reliance on fasting glucose lonely may essentially bias land-specific estimates and adversely affect planning.
Another issue demonstrates the problems researchers have in getting access to master information sources, specially from the WHO [ten]. WHO has historically not released key information related to diabetes and other not-communicable diseases that are vital for public health. Nosotros need a lot more transparency from major organizations in helping both researchers and decision makers to understand the truthful burden of diabetes, and that involves admission to the principal information. These are the barriers that we are trying to address now. Nosotros should not be using the data put out by WHO or the IDF or fifty-fifty the Global Burden of Disease Research Group [6, xi] uncritically when it comes to public wellness planning in any state, even the Us.
Epidemiological data nearly the diabetes epidemic: secular rises and falls
So what nearly this epidemic of diabetes? I started my diabetes epidemiology activities in the Pacific [12] and, later, the Indian Bounding main isle of Mauritius [13]. The inspiration for me to get into diabetes research came from the early studies of Ian Prior, a famous cardiovascular epidemiologist who, in the mid-1960s, published information about high rates of diabetes in Polynesians living in New Zealand and the Pacific islands [14]. In 1975, I was in London training at Guys Hospital and it was Christmas. It was snowing and cold and no one came to work. I was sitting there past myself and I picked upward an former British Medical Journal and read about Ian Prior's research showing high rates of diabetes in Polynesians. Subsequently Peter Bennett showed that Pima Indians living in Arizona had the highest prevalence of diabetes in any customs in the world [15]. There was too a report in Australia showing how indigenous people accept loftier rates of diabetes [xvi]. So when I returned to Australia from London, I decided to investigate the issue of diabetes in Pacific Island populations.
Our grouping "swept" through the Pacific and institute some of the highest rates of diabetes that had ever been reported [12]. This was a alert to me that we were going to face a diabetes epidemic. Indeed when nosotros did our offset Pacific survey in Republic of nauru in 1975, we found a high rate of diabetes – 34.4% in individuals >fifteen years old [17]. Peter Bennett had reported that >50% of the adult Pima Indian population over the age of 35 years had diabetes [15]. In that location was conspicuously a alarm there, and indeed, our Melbourne daily newspaper, The Age, published a alert nigh diabetes equally "The Western Killer in Paradise." Unfortunately, they put my photograph under the headline and it almost killed the point of the story!
After our grouping showed very high rates of diabetes in the Pacific, the WHO asked me to go to Mauritius to take a look at the diabetes problem in that location every bit there were some indications that diabetes was condign a problem on that beautiful and idyllic Indian Body of water Island. Information technology was important to understand diabetes in Republic of mauritius because although information technology had a relatively small population of i.2 one thousand thousand, the population represented three major ethnic groups: Asian Indians from Bharat, Creole- South African Black population, and Chinese people [13]. Together, these 3 ethnic groups stand for approximately two-thirds of the world'southward population. Whatever was happening in Mauritius could exist extrapolated to other countries where there were Indian, Chinese and Creole or Black populations.
With a squad including Sir George Alberti, a smashing bio-chemist; Jaakko Tuomilehto, whose proper noun is synonymous with the prevention of type ii diabetes; my colleagues from Australia, Jonathan Shaw and Dianna Magliano; and Sudhirsen Kowlessur from Mauritius, we have surveyed the population of Mauritius every 5 years or so from 1987 to 2015. Figure 1 shows information from Mauritius from the first written report in 1987 to the nearly recent published report from 2009 [18, 19]. Every bit yous can run into, the prevalence of diabetes went from 14.6 to 23.6%, a 62% increase over 20 years (Fig. 1a). The pattern was very similar in each ethnic group. Based on these data, we concluded that nosotros were facing a global epidemic of type 2 diabetes, particularly in countries such as China and Bharat.
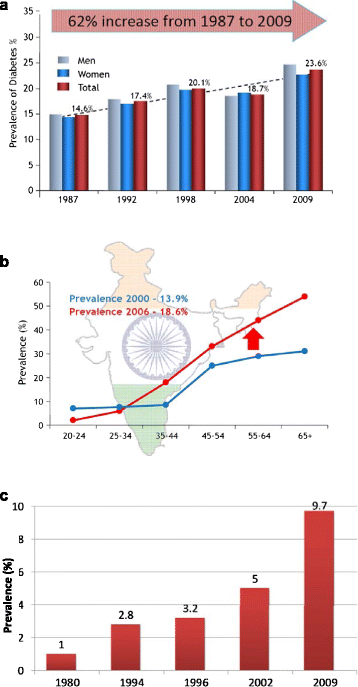
The Increase in Diabetes Prevalence in a Mauritius Adapted from [18, 19], b India Adjusted from [20], and c China Adapted from [21]
This has at present been borne out. In Bharat there has been an increment of near 5% (absolute) in diabetes prevalence betwixt the years 2000 and 2006 [20] (Fig. 1b). India now has 80–90 million people with diabetes. In India and in many heart and low-income countries, there are only non the resource to manage diabetes. In 1980, less than 1% of Chinese population had diabetes. In Beijing, the McDonalds restaurant in Tiananmen Square was ane of the busiest McDonald franchise in the world (Fig. 2). Now the estimate of diabetes prevalence in China is 9.seven% [21] (Fig. 1c). A study from Turkey has also documented an incredible 90% increase in diabetes prevalence over eleven years from 2002 to 2013 [22].
"Coca-colonization" in Prc and India. a McDonald'southward in China b Coca-cola in India
Ethnic populations are disproportionately affected by diabetes and its complications. In Australia, Indigenous populations residing in the Northern Territory have one of the highest rates of diabetes in the world and certainly amidst Indigenous communities [23]. Indigenous people in Commonwealth of australia have a four-fold higher diabetes prevalence compared to the general Australian, mainly European population. They also have the one of the highest rates of end-phase renal disease in the world [24]. Alice Springs, in the center of Australia and the home to a big Ethnic population, has the largest kidney dialysis unit in the southern hemisphere per capita, another reflection of the impact of diabetes [25]. Diabetes also impacts survival. The prevalence of diabetes falls off in the Indigenous population over 64 years of age, not because in that location is a decrease in the incidence of diabetes, merely considering of higher mortality in those with diabetes in that age category. [26].
The drivers of the type two diabetes epidemic (Tabular array 1)
In indigenous communities in Australia, as in the Usa and Canada, it is very important to understand the attitudes of affected people earlier trying to prevent or manage diabetes. We accept a "western" view that diabetes is acquired by bad beliefs, besides much sugary drinks, and eating too much. Obesity and not plenty exercise are the culprits. In contrast, the Indigenous people of Australia accept lost their lands, are in disharmony with other communities, endure from poverty and other external pressures (Table 2). Recognizing and addressing these issues is i of the greatest challenges nosotros have in trying to prevent diabetes in the communities of Australia that have the highest rates.
There are clear links amidst lifestyle, inactivity, ageing, obesity, and modernization, that contribute to diabetes. Betwixt 1980, when the first diabetes study was washed in Australia, and 2000, the prevalence of obesity almost tripled and the prevalence of diabetes increased from 2.4 to 7.two% [27] (Fig. 3). If you look at the incidence of diabetes in the Australian cohort from the year 2000, there was a 4-fold difference in risk of developing diabetes between people who were obese and those who were of normal weight [28]. Almost two-thirds of the Australian population in 2000 was overweight or obese, close to the rates of overweight and obesity in Americans.
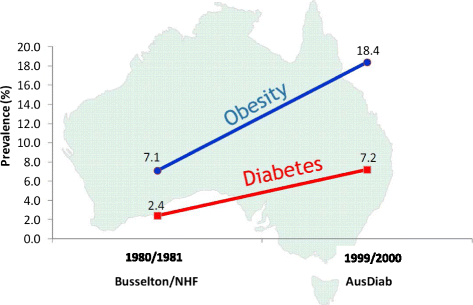
Prevalence of Diabetes and Obesity in Australia 1980/81 and 1999/2000 Adapted from [27, 28]
And then far, I've given you lot all the bad news near the epidemic of diabetes. The question is, are in that location any studies that show that the prevalence of diabetes is actually falling? Some recent data from the United states now suggest there might be a leveling off of obesity and diabetes [29]. There's some debate as to why this may exist happening; whether it is due to improved public awareness or whether everyone who is going to get diabetes already has information technology. In Republic of nauru in 1994, the prevalence of diabetes was approximately 50%. In a subsequent study almost 10 years afterwards, the rate had fallen [thirty]. Over the same time period, Nauru went from beingness the wealthiest country in the earth per capita (due to rich phosphate deposits) to one of the poorest countries in the world. So the turn down in prevalence could have been an effect of the economic collapse. Some other study reported in the British Medical Journal institute that during an economic crisis in Cuba, there was a subtract in obesity and a subtract in diabetes incidence and deaths from diabetes [31]. Then there's some testify that economic hardship may be the all-time fashion to forestall diabetes!
The prevention of type two diabetes is a major global public health challenge that we now face up. Over twenty years agone, a study by the belatedly Hilary King, an adventurous young epidemiologist, plant a 4% diabetes prevalence on a small-scale Island off of the coast of Papua New Republic of guinea [32]. This was quite high for Papua New Guinea. We considered doing a prevention written report there, simply an convulsion occurred and the whole island disappeared. I did non think it was a skillful mode to prevent diabetes, but it solved the problem there!
In 1982, Kerin O'Dea, one of our very well-known Australian diabetes investigators, took a group of Indigenous bush people for 7 weeks to live using traditional foods, such equally crocodile, kangaroo and native plants [33]. They lost weight and their glucose tolerance, insulin sensitivity, blood lipids, and blood pressure all improved (Table 3). This was one of the first demonstrations that if you return to a traditional lifestyle, you can reverse not just diabetes but other components of the metabolic syndrome. These results were extended by others including the classic study of Jaakko Tuomilehto, the Finnish Diabetes Prevention Study [34]. He observed a reduction of 58% in the risk of progression to type 2 diabetes; this now seems to exist an accepted consequence at present amidst persons at loftier-risk people of diabetes.
Epigenetics and run a risk for diabetes
Although I have always been a strong laic in the "CocaColonization" story, a term suggested by Arthur Koestler [35], that changes of lifestyle in rural and traditional island populations accept caused the epidemics of obesity and diabetes, I recollect in that location are emerging data that suggest we demand to rethink the story and consider the impact of epigenetics. In 1990, David J. P. Barker first proposed that in utero metabolic adaptation defines a trajectory of growth that prepares the fetus for its likely developed environment [36]. What happens in utero to the fetus depends on the mother's and the begetter'due south behaviors earlier formulation and the mother's during pregnancy. The story goes back to the Dutch wintertime famine [37]. At the end of World War 2, there was a famine during the Nazi Germany occupation of Holland. Women who were significant were on very poor diets. Some 30 years later on, researchers looked to see what happened to the children who were born at that time. They found loftier rates of diabetes, obesity, hypertension, and indeed some mental disorders like schizophrenia in the offspring of women who were undernourished during early pregnancy. This raised the issue of the famine and what happened many years afterward when these children became adults. Their risks of chronic diseases were increased.
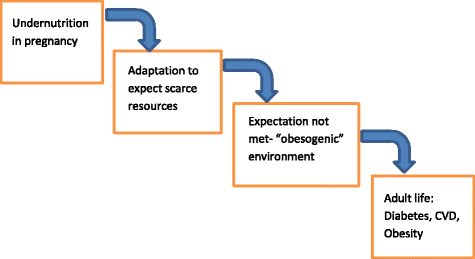
Another example occurred during the Chinese famine of 1958–1962 [38]. In that location was near minimal diabetes in Prc before 1980 [39]. Some 30–forty years later that dearth, there are now over 120 million Chinese with diabetes [40]. Again, this raises a question of the office of a famine and the effect of the famine on children exposed to intrauterine undernutrition. In very unproblematic terms, epigenetics reflects not a change in the genes of the fetus, but a change in the DNA effectually the genes. That DNA influences how the gene reacts with potential environmental risk factors including those noted in the figure (Fig. 4). This can also happen to children born during a dearth so that 20–30 years subsequently, when they come into an obesogenic environment, they get diabetes.

Developmental plasticity, fetal programming and intergenerational risk
This is just an instance of some of the hazard factors that can influence in utero this procedure and it'southward been well demonstrated in beast studies that this happens. All of the data so far in humans is retrospective, but there is at present a prospective study in Singapore led by Professor Sir Peter Gluckman, to assess the impact of epigenetics at a human level [41]. What is also interesting is that diabetes itself is one of the many factors that tin can cause epigenetic changes. We know that mothers with pre-gestational diabetes and mothers with gestational diabetes are more likely to have offspring who are either obese or have diabetes. And the epigenetic event appears to be intergenerational. It means you could have a barbarous bike perpetuating the diabetes epidemic. Gluckman and Hansen have authored a book, Mismatch [42], suggesting that a baby built-in in a famine state of affairs expects to come up out into the dearth, only may arrive into an obesogenic environment. I have tried to make this phenomenon a piddling clearer by pointing out that with undernutrition in pregnancy, the adaptation is to wait a scarce resources environment. If the expectation is not met considering the infant arrives to an obesogenic environment, nosotros may see both early changes in the child, and an increased chance of obesity, diabetes, and center disease in adult life (Fig. v).
Mismatch: The relevance for prevention of blazon 2 diabetes
I think this is a real story. College rates of diabetes likewise may be linked to famine situations that occurred in the Ukraine (1932–1933) [43] and in Cambodia (1975–79) [44, 45]. We now have a famine in the Horn of Africa. This raises very important issues equally to how the United Nations (Un), the WHO, and the UN Evolution Program and other NGOs handle food relief during and after a dearth. These may be very important aspects of preventing diabetes in communities many, many years hence. So finally the message is out to be very wary of national and international predictions of this diabetes epidemic. We need to exist looking more than closely at maternal and child health, and the whole issue of early on development in utero to reduce the take a chance to time to come generations. The next epidemic may occur in countries in the Horn of Africa if nosotros exercise non pay attending to the correct way of treatment the nutritional and social problems particularly with aid and nutrient supplies.
Source: https://clindiabetesendo.biomedcentral.com/articles/10.1186/s40842-016-0039-3
0 Response to "Risk of Developing Diabetes in Individuals With Family History of Diabetes"
Post a Comment